By Brad G. Philbrick, RPh
I remember the patient clearly—a man in his mid-forties who came to the counter with a familiar look of fatigue and frustration. He had been prescribed antibiotics for a respiratory infection but returned a week later, coughing again and asking if the same medication could be refilled. I looked at his profile, then at him, and asked gently, “Did you finish the full prescription?”
He hesitated, shifting his weight. “Well,” he said, “I stopped after five days when I felt better. I figured I didn’t need the rest.”
It was an exchange I’d had more times than I can count over my years behind the pharmacy counter. I explained, once again, that antibiotics are not pain relievers or symptom soothers—they are tools of precision meant to eliminate bacteria fully. Stopping early leaves the strongest bacteria alive, the ones clever enough to survive and replicate. Those surviving microbes learn. And they don’t forget.
I saw this pattern too many times: infections that returned stronger, more resistant, more dangerous. It was disheartening because every relapse was a reminder that medicine, no matter how advanced, still relies on partnership between patient and prescriber—trust, understanding, and follow-through.
Antibiotics are among the greatest gifts of modern medicine. Penicillin, discovered by Alexander Fleming in 1928, changed the world almost overnight. Infections that once meant certain death became curable. Pneumonia, strep throat, tuberculosis, even infected wounds—what was once feared became treatable.
Yet, over the decades, we’ve taken that miracle for granted. We’ve come to see antibiotics as quick fixes—something to request “just in case,” even for viral infections like colds or the flu, where they have no benefit at all. And when symptoms fade, we often assume we’re healed, leaving half-filled bottles behind.
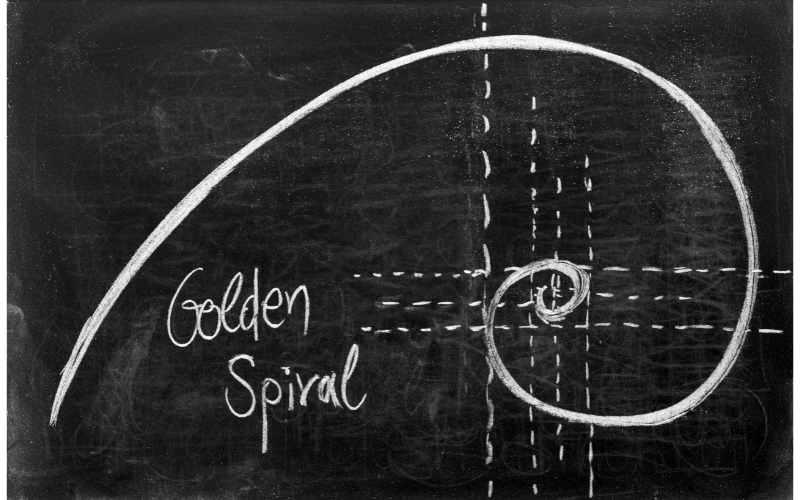
The truth is that bacteria are far from passive. They evolve, adapt, and develop resistance. Each time an antibiotic course is cut short, it’s like calling off the battle just as the enemy retreats, leaving a few survivors to regroup—and come back stronger.
The Centers for Disease Control and Prevention estimates that in the U.S. alone, more than 2.8 million infections each year are caused by antibiotic-resistant bacteria, leading to over 35,000 deaths. Globally, that number exceeds a million. The rise of so-called “superbugs” is not a distant medical problem—it’s a direct consequence of how we, collectively, use (and misuse) these powerful drugs.
In hospitals and clinics, antibiotic stewardship refers to coordinated efforts that ensure these medications are used only when needed, in the right doses, and for the proper duration. But stewardship doesn’t stop at the hospital door. It’s a shared responsibility between healthcare providers and the public.
For pharmacists like me, stewardship means guiding patients to understand their treatment—not just dispensing a pill bottle, but offering context, encouragement, and accountability. For patients, it means honoring the course of therapy, even when they feel better, because the healing process continues beyond visible symptoms.
Each person who completes an antibiotic regimen contributes to the collective effort to preserve these medicines for future generations. Each person who resists the urge to save “a few for next time” plays a part in slowing resistance. And each person who trusts their healthcare provider’s advice helps ensure that antibiotics remain potent allies, not compromised relics.
I’ve seen patients cry tears of relief when an infection cleared and their strength returned. I’ve also seen the anguish of those who relapsed because a few pills were left untouched. It’s never just about compliance—it’s about connection, communication, and shared responsibility.
When we talk about antibiotic stewardship, we’re really talking about the stewardship of healing itself: a moral and medical responsibility to respect the medicines that respect us back.
The power of antibiotics lies not only in chemistry but in cooperation. Healing is not something medicine does to us—it’s something we do with it.
So the next time you’re prescribed antibiotics, remember that finishing the bottle isn’t just about feeling better today. It’s about ensuring that medicine remains capable of healing tomorrow.
References
- Centers for Disease Control and Prevention (CDC). Antibiotic Resistance Threats in the United States, 2024.
- World Health Organization (WHO). Global Action Plan on Antimicrobial Resistance.
- Mayo Clinic. Antibiotic Stewardship: Protecting the Power of Antibiotics.
- The Lancet Infectious Diseases (2023). Global Burden of Bacterial Antimicrobial Resistance in 204 Countries and Territories.